Creasy And Resnick Pdf Free
Posted : admin On 01.09.2019An abnormally adherent placenta occurs when a defect in the endometrial lining that lies under the placenta ( the decidua basalis) allows the placenta to grow to varying depths. Beyond the lining of the uterus (endometrium) into or through the myometrium (wall of the uterus) and sometimes into the adjacent bladder and intestines. At delivery the placenta fails to separate from the uterine wall. Manual attempts to remove the placenta may cause profuse hemorrhage. The condition is collectively referred to as “placenta accreta”.
The three types of abnormally adherent placenta are defined according to the depth of invasion by the placenta into the myometrium. 1. Placenta accreta: The placenta grows superficially into the myometrium (muscular wall of the uterus). This is the most common form of an abnormally adherent placenta and occurs in 75% of cases. Placenta increta: The placenta grows into the myometrium. This occurs in 18% of cases. Placenta percreta.
If searching for the ebook Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice: Expert Consult Premium Edition - Enhanced Online Features and Print, 7e by Robert K. Creasy MD;Robert Resnik MD;Jay D. Iams MD in pdf form, then you have come on to correct site. Get this from a library! Creasy and Resnik's maternal-fetal medicine: principles and practice. Robert K Creasy; Robert Resnik; Michael F Greene; Jay D Iams; Charles J Lockwood; - In your practice, you require advanced knowledge of the obstetrical, medical, genetic and surgical complications of pregnancy and their effects on the mother and fetus.
The placenta grows completely through the uterus and may invade surrounding structures such as the bladder.and bowel. Fortunately, this is the least common form and occurs in about 7% of cases LifeArt Image copyright 2007.Modified by Focus I.T.2014 RISK FACTORS The most important risk factor for the development of placenta accreta appears to be placenta previa. Patients presenting with a placenta previa and an unscarred uterus have a 5% risk of clinical placenta accreta. The incidence of placenta accreta increases to 24% in women with a placenta previa and one previous cesarean section.
The risk continues to increase with each additional cesarean section up to 67% in women with a placenta previa and four or more cesarean sections 4. Placenta Previa with Prior Uterine Incisions: Effect on Incidence of Placenta Accreta Number of Prior Uterine Incisions Percent with Placenta Accreta 0 5 1 24 2 47 3 40 4 67 Clark SL, Koonings PP, Phelan JP. Placenta previa/accreta and prior cesarean section. Obstet Gynecol 1985 Jul;66(1):89-92 Other risk factors that have been associated with the development of placenta accreta include 6:. A history of myomectomy. Asherman syndrome. Previous uterine thermal ablation,.
Uterine artery embolization. Maternal age greater than 35 years old,. Second-trimester serum levels of AFP and free beta-hCG greater than 2.5 multiples of the median EVALUATION Placenta accreta should be suspected in all women with placenta previa or when the placental location overlies a previous uterine scar. Ultrasound 2. “Grayscale ultrasonography is sensitive (77–87%) and specific (96–98%) for the diagnosis of placenta accreta The presence and increasing number of lacunae within the placenta at 15–20 weeks of gestation have been shown to be the most predictive ultrasonographic signs of placenta accreta”.
Additional findings on grayscale ultrasonography that suggest placenta accreta is present include 7: ● abnormal placental lacunae.
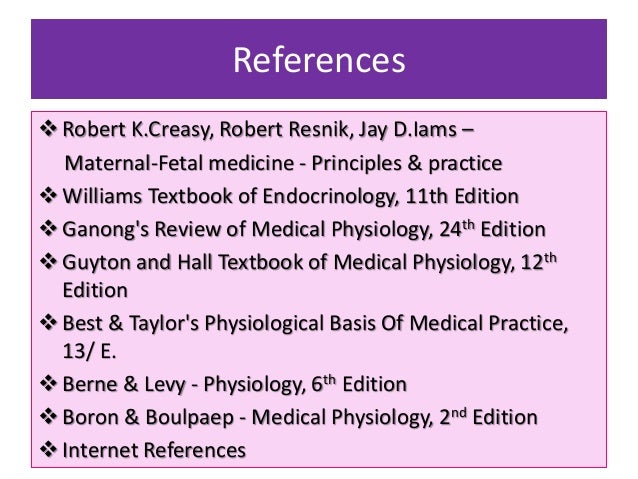
Minimize complications with Creasy and Resnik's Maternal-Fetal Medicine.This medical reference book puts the most recent advances in basic science, clinical diagnosis, and management at your fingertips, equipping you with the up-to date evidence-based guidelines and knowledge you need to ensure the best possible outcomes in maternal-fetal medicine. Creasy & Resnik’s Maternal-Fetal Medicine: Principles and Practice remains an authoritative reference book for clinical residents, fellows and practicing specialists in Maternal-Fetal Medicine.' Reviewed by Ganesh Acharya, Feb 2015 Key Features. Part 1: Scientific Basis of Perinatal Biology 1. Human Basic Genetics and Patterns of Inheritance 2. Normal Early Development 3.
Amniotic Fluid Dynamics 4. Multiple Gestation: The Biology of Twinning 5. Biology of Parturition 6. Immunology of Pregnancy 7. Maternal Cardiovascular, Respiratory and Renal Adaptation to Pregnancy 8. Endocrinology of Pregnancy 9. The Breast and Physiology of Lactation 10.
Creasy And Resnick Pdf Free Software
Maternal Nutrition 11. Developmental Origins of Health and Disease 12. Fetal Cardiovascular Physiology 13. Behavioral State in the Fetus: Relationship to Fetal Health and Development 14. Placental Respiratory Gas Exchange and Fetal Oxygenation 15. Fetal Lung Development and Surfactant 16.
This gives me a thorough listing of the server’s hardware but, in this case, the site returned nothing that I didn’t already know. Figure 2 – Determining hardware specs from the BIOS utility – The next step is to use the and not surprisingly, the server isn’t listed here either. Well, let’s try and plug in the serial number on HP’s support. 2, the BIOS utility is of very little help save for the processor type and serial number provided. Vmware 6 download.
Evidence-Based Practice in Perinatal Medicine Part 2: Obstetrical Imaging Section I Principles of Fetal Imaging 17. Performing and Documenting the Fetal Anatomy Ultrasound Examination 18. Doppler Ultrasound: Select Fetal and Maternal Applications 19. Clinical Applications of Three-Dimensional Sonography in Obstetrics Section II Lesions 20. Central Nervous System Imaging 20A: Cephalocele 20B: Choroid Plexus Cysts 20C: Holoprosencephaly 20D: Porencephalic Cyst 20E: Encephalocele 20F: Ventriculomegaly: Aqueductal Stenosis 20G: Ventriculomegaly: Arnold-Chiari Malformation 20H: Ventriculomegaly: Dandy Walker Malfromation and Variant 20I. Agenesis of the Corpus Callosum (online only) 20J. Anencephaly (Online only) 20K.
Arachnoid Cyst (Online only) 20L. Hydranencephaly (Online only) 20M. Microcephaly (Online only) 20N.
Vein of Galen Aneurysm (Online only) 21. Imaging of the Face and Neck 21A: Cleft Lip and Palate 21B: Cystic Hygroma 21C: Micrognathia 21D: Abnormal Orbits (Online only) 21E: Goiter (Online Only) 22. Thoracic Imaging 22A: Congenital Diaphragmatic Hernia 22B: Cystic lung lesions, CCAM, Sequestration 22C: Congenital High Airway Obstruction (CHAOS) (Online only) 22D: Pleural Effusion (Online Only) 23. Fetal Cardiac Malformations and Arrhythmias: Detection, Diagnosis, Management, and Prognosis 24. Abdominal Imaging 24A.
Abdominal Ascites 24B. Cystic Abdominal Lesions 24C.
Echogenic Abdominal Lesions 24D. Gastroschisis 24E. Intestinal Atresias 24F. Omphalocele 24G. Esophageal Atresia (Online only) 24H. Limb-Body Stalk Anomaly (Online only) 24I. Umbilical Vein Varix (Online only) 25.
Urogenital Imaging 25A. Bladder Exstrophy 25B. Echogenic Dysplastic Kidneys 25C.
Multicystic Kidney 25D. Posterior Urethral Valves 25E. Pyelectasis 25F. Ureterocele 25G. Ambiguous Genitalia (online only) 25H. Duplicated Renal Collecting System (online only) 25I. Renal Agenesis (online only) 25J.
Creasy Greens
Ureterovesical Junction Obstruction (online only) 26. Skeletal Imaging 26A. Arthrogryposis and Polydactyly 26B. Clubfoot 26C.
Neural Tube Defect 26D. Sacrococcygeal Teratoma and Sacral Agenesis 26E.
Skeletal Dysplasia 26F. Amniotic Band Syndrome (online only) 26G. Craniosynostosis and Cloverleaf Skull (online only) 26H. Hemivertebrae and Scoliosis (online only) 27. Imaging of the Placenta and Umbilical Cord 27A.
Marginal and Velamentous Umbilical Cord 27B. Molar Gestation 27C. Placenta Accreta-Increta-Percreta 27D. Placental Echolucencies: lakes, Cysts, Chorangionma 27E. Placenta Previa 27F. Single Umbilical Artery 27G.
Circumvallate Placenta (online only) 27H. Subchorionic Hematoma (online only) 27I. Succenturiate Placenta (online only) 27J. Vasa Previa (online only) 28. Uterus and Adnexae Imaging 28A. Adnexal Mass, Complex and Simple 28B.
Amniotic Fluid Volume 28C. Uterine Anomalies 28D. Uterine Fibroids 29. First Trimester 29A.
Anomalies 29B. Nuchal Translucency 29C. Nasal Bone (online only) Part 3: Fetal Disorders: Diagnosis and Therapy 30. Prenatal Diagnosis of Congenital Disorders 31. Teratogenesis and Environmental Exposure 32. Assessment of Fetal Health 33. Intrapartum Fetal Surveillance 34.
Assessment and Induction of Fetal Pulmonary Maturity 35. Invasive Fetal Therapy 36.
Hemolytic Disease of the Fetus and Newborn 37. Nonimmune Hydrops 38. Multiple Gestation: Clinical Characteristics and Management Part 4: Disorders at the Maternal-Fetal Interface 39. Pathogenesis of Spontaneous Preterm Birth 40. Preterm Labor and Birth 41. Cervical Insufficiency 42. Premature Rupture of the Membranes 43.
Clinical Aspects of Normal and Abnormal Labor 44. Recurrent Pregnancy Loss 45. Stillbirth 46. Placenta Previa, Placenta Accreta, Abruptio Placenta, and Vasa Previa 47. Intrauterine Growth Restriction 48. Pregnancy-Related Hypertension Part 5: Maternal Complications 49. Patient Safety in Obstetrics 50.
Maternal Mortality 51. Maternal and Fetal Infections 52. Cardiac Diseases 53. Coagulation Disorders in Pregnancy 54. Thromboembolic Disease in Pregnancy 55. Anemia and Pregnancy 56. Malignancy and Pregnancy 57.

Renal Disorders 58. Respiratory Diseases in Pregnancy 59. Diabetes in Pregnancy 60. Thyroid Disease and Pregnancy 61. Other Endocrine Disorders of Pregnancy 62. Gastrointestinal Disease in Pregnancy 63.
Diseases of the Liver, Biliary System, and Pancreas 64. Pregnancy and Rheumatic Diseases 65. Neurologic Disorders 66. Management of Depression and Psychoses in Pregnancy and the Puerperium 67.
Substance Abuse in Pregnancy 68. The Skin and Pregnancy 69.
Benign Gynecological Conditions in Pregnancy 70. Anesthesia Considerations for Complicated Pregnancies 71. Intensive Care Considerations for the Critically Ill Parturient Part 6: The Neonate 72. Neonatal Morbidities of Prenatal and Perinatal Origin.